The 2025 breakout medical drama, The Pitt, received overwhelmingly positive reviews from healthcare workers for its realistic portrayal of an emergency department (ED) over a tumultuous 15-hour shift. Among the important, real-world issues presented by the show was one common scenario that every ED provider in the United States recognized.
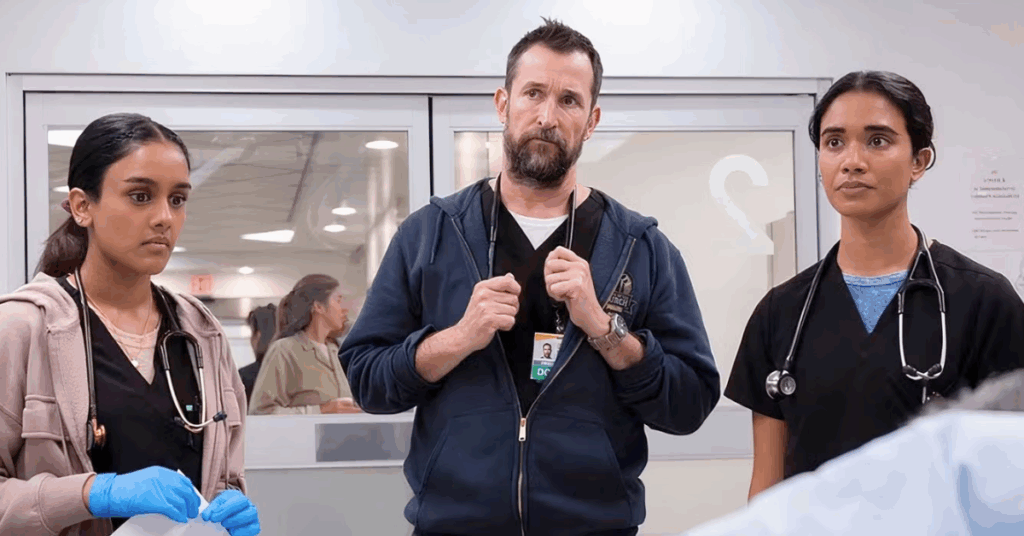
In the series premiere, a patient arrives in an ambulance with a life-threatening injury. After Dr. Robby, a courageous attending physician played by ER’s Noah Wyle, and his team stabilize the patient, they quickly determine that no one knows what language she is speaking.
Patients with limited English proficiency (LEP) interact with healthcare systems differently than their English-speaking peers, often experiencing delayed access and worse outcomes. Medical interpreters are an integral part of the lifesaving work in EDs across the country, providing vital bridges to communication that enable providers to deliver the best possible patient care.
As linguists and partners in language access, we were thrilled to see The Pitt bring visibility to the needs of LEP patients and offer a window into the dynamic challenges faced by emergency department providers. Their commitment is nothing short of heroic. Here, we examine the impact of this LEP patient’s storyline and explore what it takes to ensure LEP patients receive support when they visit the emergency room.
There Are More Than 25 Million LEP Patients in the United States
According to the U.S. Census Bureau’s 2022 American Community Survey, more than 25 million people in the United States are limited English proficient. This population is growing, yet studies continue to show that LEP patients experience worse health outcomes on average.
Between lower rates of healthcare coverage among immigrant populations, language barriers with healthcare providers, and challenges with managing chronic conditions, LEP patients are vulnerable. When we work together to uplift the care and experiences of LEP patients in times of crisis, our neighborhoods and communities benefit exponentially.
Other studies have shown the impact of language barriers on hospital resources. Providers may feel more comfortable ordering additional tests or observing LEP patients over longer stays. These additional measures (and costs) may not be necessary if a qualified medical interpreter is available to assist with communication.
Language Access Supports LEP Patients in Emergency Rooms
Viewers and critics of The Pitt witness compassion and competence unfold in the fictional Pittsburgh Trauma Medical Center, and real-world healthcare workers say the portrayal rings true. It is the providers’ persistence and dedication that impressed audiences, while physicians and nurses found the medicine, pace, and colleague relationships to reflect their lived experiences in the ED.
Supporting LEP patients in emergency rooms requires close coordination and a clear process for locating interpreters. From our perspective, The Pitt handles this sensitive matter accurately. There isn’t much else Dr. Robby and his team can do to identify this LEP patient’s spoken language sooner, who arrives with a level one triage injury and a pain level that makes communication next to impossible. The language barrier likely goes unnoticed during the ambulance ride.
Once the patient’s condition is better managed, Dr. Robby leaves to contact language services—the correct action to take on behalf of an LEP patient. Later in the series, viewers discover that she speaks Nepali, and our heroic providers have activated a tried-and-true solution, especially for less commonly spoken languages: video remote interpreting (VRI). Viewers see the patient and providers communicate with the help of a Nepali-speaking interpreter through a portable, video-enabled device. The patient is on the road to recovery.
According to the Pew Research Center, there may be as many as 5,000 Nepali-speaking individuals in Pittsburgh, or less than 0.02% of the city’s population. While the numbers tell one story, the reality is altogether different. Regardless of national origin or size, every community needs access to emergency healthcare services. Language access significantly reduces harm, suffering, and loss of life, especially considering that VRI can provide coverage for most major languages.
Language Access in Hospitals Helps Providers Focus on the Medicine
The Pitt also reminds audiences to consider the vital role of nurses in hospital operations. Pittsburgh Trauma Medical Center clearly could not run without them.
Princess (Kristin Villanueva) and Perlah (Amielynn Abellera) perform challenging, hands-on tasks over their 15-hour shift, often sidebarring in Tagalog in moments of reprieve. Princess and Perlah offer a window into the experiences of the more than 150,000 Filipino nurses who have immigrated to the United States since 1960.
While nurses are an irreplaceable addition to any emergency department team, even multilingual nurses cannot replace the role of language access in hospitals. Between intakes and discharges, medicine management, coordinating with other departments, and plenty of other tasks, nurses’ obligations are nonstop. There is hardly room for on-call interpretation. Instead, the most effective way to support emergency department staff communication with LEP patients is through dedicated language access professionals.
Even as emotions run high and interpersonal disagreements simmer beneath the surface, The Pitt’s Dr. Robby and his staff function like a well-oiled machine. Small actions, such as calling an interpreter, can make all the difference to a patient who cannot communicate with doctors and nurses. This positive patient outcome was no accident. Viewers can assume that Pittsburgh Trauma Medical Center has a language access plan that explains how to deploy language services, lays out staff protocols, analyzes LEP patient feedback, and identifies opportunities for improvement.
In the case of their Nepali-speaking patient, Dr. Robby or Dana might consider asking the hospital’s language access manager to explore strategies for language identification before a patient reaches the ED. Perhaps the local paramedic team would benefit from a refresher training. Also, new technologies are emerging that can recognize spoken languages, reducing confusion and enabling providers to call on the right interpreter at the right time. This type of forethought streamlines patient experiences, allowing providers to remain focused on the medicine and saving lives.
Improving Patient Experiences with PGLS Interpreters
If you want to explore opportunities to support LEP patients in emergency rooms, our free eBook details the processes and considerations of building a comprehensive language access plan. As a strategic partner to hospital networks, PGLS provides valuable planning assistance and VRI services in over 100 languages and regional varieties. Get in touch to learn more.